Healthcare revenue cycle management represents the financial heartbeat of any medical practice or healthcare organization. From the moment a patient schedules an appointment to the final payment collection, every step in this process affects your bottom line and operational efficiency.
The complexity of healthcare RCM has grown significantly over the years. You're not just dealing with patient care anymore - you're navigating insurance verification, prior authorizations, complex coding requirements, denial management, and constantly changing reimbursement rules. Each missed step can cost your practice thousands of dollars in lost revenue.
What makes healthcare revenue cycle management different from other industries is the intricate relationship between clinical care and financial processes. Unlike retail businesses where payment happens at the point of sale, healthcare providers must deliver services first, then navigate a complex billing and reimbursement process that can take months to complete.
The stakes are high too. Poor RCM processes can lead to cash flow problems, increased denials, compliance issues, and ultimately threaten the financial sustainability of your practice. That's why understanding and optimizing your revenue cycle has become critical for healthcare success.
The revenue cycle begins before the patient even walks through your door. Accurate patient registration and thorough insurance verification form the foundation of successful RCM processes. When this step is done correctly, it prevents countless downstream issues that could delay or prevent payment.
During registration, your team needs to collect complete demographic information, insurance details, and verify coverage for the planned services. This includes checking patient eligibility, understanding benefit limitations, and identifying any prior authorization requirements.
Insurance verification isn't a one-time activity either. Patient insurance status can change frequently, so verification should happen at every visit. Many practices implement automated eligibility checking systems that verify insurance coverage in real-time, reducing the risk of treating patients with inactive or changed coverage.
The goal is ensuring that you have all the information needed to bill correctly the first time. Clean claims start with clean data, and clean data starts with thorough patient registration and verification processes.
Accurate medical coding serves as the bridge between clinical care and financial reimbursement. Your coding team must translate complex medical services into standardized codes that insurance companies can process and pay. This translation must be precise because coding errors are one of the leading causes of claim denials.
The coding process requires deep understanding of medical procedures, diagnosis codes, and ever-changing coding guidelines. Coders must stay current with updates to ICD-10, CPT, and HCPCS codes while ensuring that all services are properly documented and coded according to payer requirements.
Documentation quality directly impacts coding accuracy. Physicians and clinical staff need to provide detailed, specific documentation that supports the codes being submitted. Vague or incomplete documentation leads to coding challenges, potential compliance issues, and delayed reimbursements.
Many healthcare organizations invest in ongoing coding education and regular audits to maintain accuracy. The cost of proper training and quality assurance is far less than the revenue lost from coding errors and denials.
Once coding is complete, claims must be submitted to payers in a timely and accurate manner. The claims process involves formatting information correctly, including all required documentation, and submitting through the appropriate channels for each payer.
Electronic claim submission has become the standard because it's faster and more efficient than paper claims. However, electronic submission requires careful attention to payer-specific formatting requirements and submission guidelines. Each insurance company may have different requirements for claim submission.
The key to successful claim submission is establishing standardized processes that ensure consistency and accuracy. This includes pre-submission claim scrubbing to identify potential errors before claims are sent to payers, reducing the likelihood of denials and accelerating payment.
Timing also matters significantly in claim submission. Most payers have specific timeframes for claim submission, and late claims may be automatically denied. Efficient RCM systems track these deadlines and ensure timely submission of all claims.
.png)
Even with perfect processes, some claim denials are inevitable. The difference between successful and struggling healthcare organizations often lies in how effectively they handle denials. Proper denial management can recover significant revenue that would otherwise be lost.
Effective denial management starts with categorizing denials by root cause. Some denials are simple administrative errors that can be quickly corrected and resubmitted. Others require clinical documentation or appeals that may take weeks or months to resolve.
The most successful practices implement denial prevention strategies alongside denial management. By analyzing denial patterns, they identify common causes and implement process improvements to prevent similar denials in the future. This proactive approach is more cost-effective than constantly fighting denials after the fact.
Appeals processing requires specialized knowledge of payer policies and regulations. Staff must understand when appeals are appropriate, what documentation is required, and how to present compelling cases for overturning denials. This specialized knowledge often justifies dedicated denial management resources.
Modern healthcare RCM relies heavily on technology to manage the complexity and volume of financial transactions. From electronic health records to automated billing systems, technology integration can significantly improve efficiency and accuracy throughout the revenue cycle.
Practice management systems provide the backbone for most RCM operations, handling patient scheduling, registration, charge capture, and billing processes. These systems must integrate seamlessly with clinical systems to ensure that all billable services are captured and coded correctly.
Automation can handle many routine RCM tasks, from insurance verification to claim submission and payment posting. This automation reduces manual errors and frees staff to focus on more complex tasks that require human judgment and expertise.
However, technology is only as good as the processes it supports. Successful RCM technology implementation requires careful workflow design, thorough staff training, and ongoing optimization to ensure that technology enhances rather than complicates revenue cycle operations.
You can't improve what you don't measure. Successful healthcare revenue cycle management requires comprehensive performance monitoring and analytics to identify opportunities for improvement and track progress over time.
Key performance indicators for RCM include days in accounts receivable, clean claim rates, denial rates, collection percentages, and cost to collect. These metrics provide insights into different aspects of revenue cycle performance and help identify areas that need attention.
Analytics should go beyond basic reporting to include trend analysis, benchmarking against industry standards, and predictive modeling to identify potential issues before they impact performance. Many organizations use dashboard reporting to provide real-time visibility into RCM performance.
The goal is creating a data-driven culture where decisions are based on objective performance metrics rather than assumptions or anecdotal evidence. This approach leads to more effective process improvements and better financial outcomes.
Your RCM team is your most valuable asset in achieving financial success. Investing in comprehensive training and ongoing development ensures that staff have the knowledge and skills needed to handle complex revenue cycle challenges effectively.
Training programs should cover both technical skills like coding and billing procedures, as well as soft skills like customer service and communication. Staff need to understand not just how to perform their tasks, but why these processes matter and how they contribute to overall practice success.
Regular training updates are essential because healthcare regulations, coding guidelines, and payer policies change frequently. Staff must stay current with these changes to maintain accuracy and compliance in their work.
Cross-training is also valuable because it creates flexibility in staffing and ensures that critical functions can continue even when key employees are unavailable. This redundancy protects against disruptions that could impact cash flow.
Healthcare RCM operates in a highly regulated environment where compliance failures can result in significant penalties. Regular quality assurance and compliance monitoring help identify and correct issues before they become serious problems.
Quality assurance should include regular audits of coding accuracy, billing practices, and documentation quality. These audits help identify training needs, process improvements, and potential compliance risks.
Compliance monitoring involves staying current with changing regulations and ensuring that RCM processes align with current requirements. This includes understanding fraud and abuse regulations, privacy requirements, and payer-specific policies.
Many organizations implement ongoing compliance training and regular policy updates to ensure that all staff understand their responsibilities and the importance of maintaining compliance in all RCM activities.
The patient experience is an increasingly important component of successful revenue cycle management. Clear communication about financial responsibilities, payment options, and billing processes improves patient satisfaction and payment collection rates.
Financial counseling should begin before services are provided, helping patients understand their insurance benefits, out-of-pocket responsibilities, and payment options. This proactive communication prevents surprises and improves the likelihood of payment.
Patient payment plans and financial assistance programs can help patients manage their healthcare expenses while ensuring that providers receive payment for services. These programs require careful administration but can significantly improve collection rates.
Clear, understandable billing statements and responsive customer service also contribute to better patient relationships and improved collection outcomes. Patients who understand their bills and feel treated fairly are more likely to pay promptly.
.png)
Q: What is healthcare revenue cycle management and why is it important?
A: Healthcare revenue cycle management (RCM) encompasses all administrative and clinical functions that capture, manage, and collect patient service revenue. It's crucial because it directly impacts cash flow, operational efficiency, and the financial sustainability of healthcare organizations.
Q: What are the main stages of the healthcare revenue cycle?
A: The main stages include patient registration and insurance verification, charge capture and coding, claim submission, payment posting, denial management, and patient collections. Each stage must function effectively for optimal financial performance.
Q: How can healthcare organizations reduce claim denials?
A: Reducing denials requires accurate patient registration, thorough insurance verification, proper coding and documentation, clean claim submission, and proactive denial prevention programs that address common causes of denials before they occur.
Q: What role does technology play in modern RCM?
A: Technology automates routine tasks, improves accuracy, enhances workflow efficiency, and provides analytics for performance monitoring. Key technologies include practice management systems, automated eligibility checking, claim scrubbing software, and business intelligence tools.
Q: How should healthcare practices measure RCM performance?
A: Important metrics include days in accounts receivable, clean claim rates, denial rates, collection percentages, cost to collect, and patient satisfaction scores. Regular monitoring of these KPIs helps identify improvement opportunities and track progress.
Q: What are common RCM challenges facing healthcare organizations?
A: Common challenges include increasing claim denials, complex payer requirements, staffing shortages, technology integration issues, changing regulations, patient financial responsibility growth, and the need to balance cost control with quality patient care.
Q: Should healthcare practices outsource RCM or keep it in-house?
A: The decision depends on practice size, complexity, available resources, and strategic priorities. Outsourcing can provide expertise and technology access, while in-house operations offer more control. Many organizations use hybrid approaches combining internal oversight with external support.
Q: How often should RCM processes be reviewed and updated?
A: RCM processes should be reviewed quarterly with comprehensive annual assessments. However, specific components like payer policies and coding guidelines require ongoing monitoring as they change frequently throughout the year.

A practical comparison of hiring a freelancer vs using a dedicated offshore accounting team, focusing on continuity, quality control, security, and scaling.
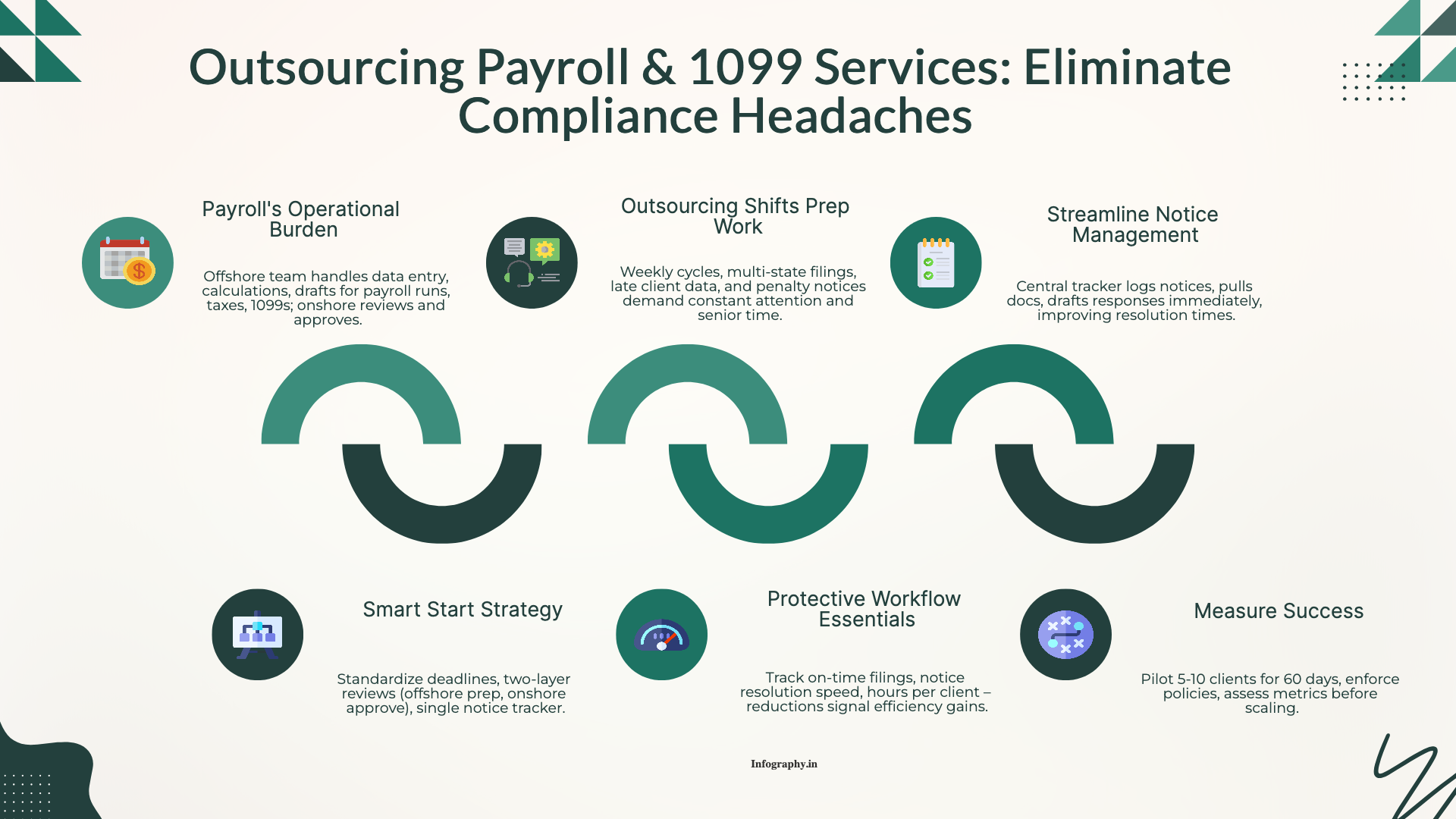
How CPA firms outsource payroll and 1099 work to reduce penalties and admin load, with a clean workflow for approvals, filings, and year-end reporting.
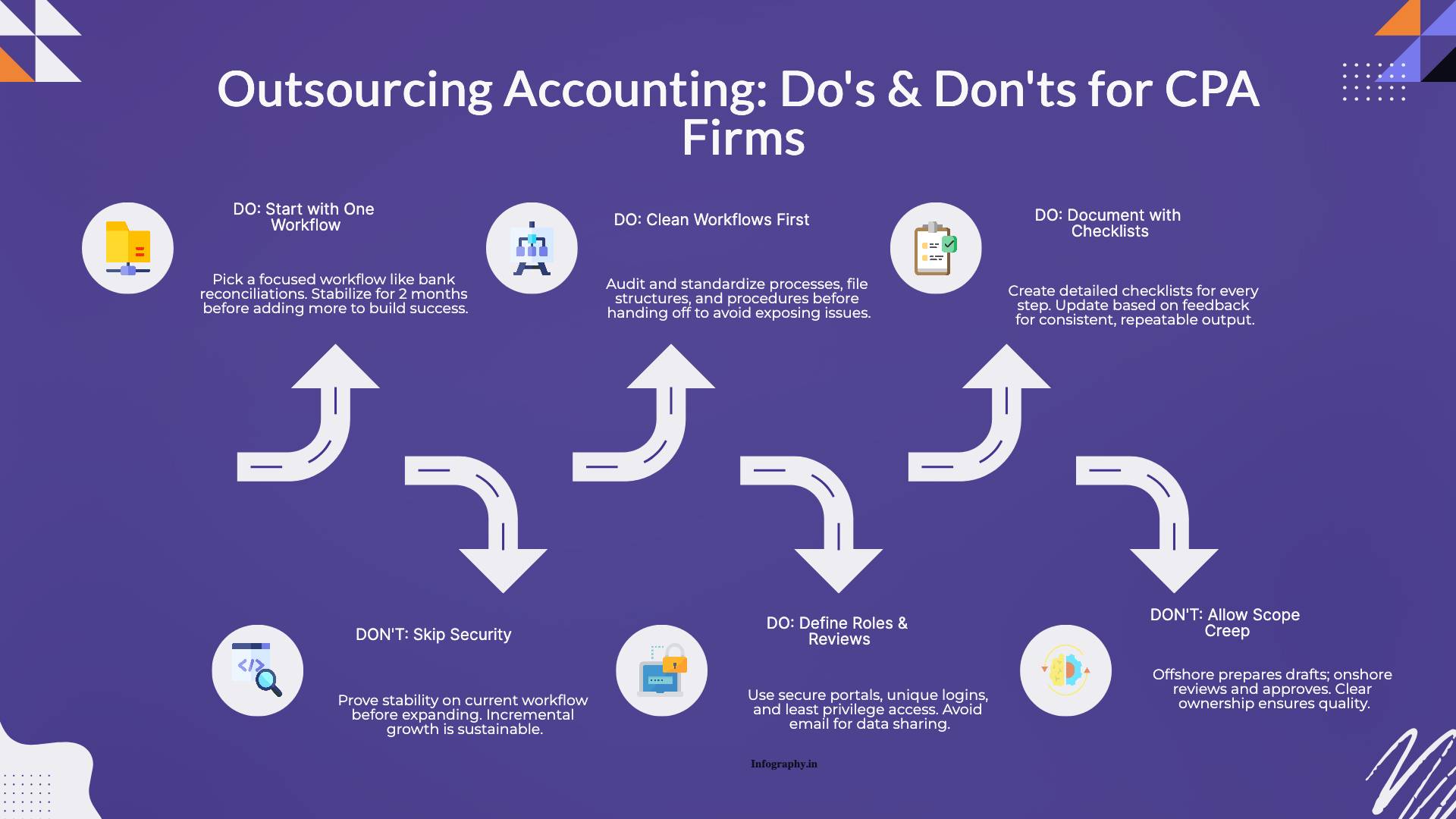
Practical do's and don'ts for CPA firms outsourcing accounting work, based on common failure points and what successful rollouts do differently.