Medical practices face a unique intersection of healthcare delivery, business management, and regulatory compliance. Whether you operate a solo practice, multi-specialty group, or outpatient clinic, financial management cannot be an afterthought. Rising costs, insurance reimbursements, complex payroll structures, and shifting regulations require dedicated accounting systems tailored to the healthcare industry.
Standard bookkeeping practices may fail to capture the nuance of medical operations. From reconciling insurance payments to managing physician compensation models, medical practice accounting demands precision and industry awareness that helps healthcare professionals streamline their financial operations.
A qualified CPA with healthcare experience can provide consultation services that go far beyond basic accounting, offering strategic guidance that allows medical practices to focus on patient care while maintaining financial health.
In this guide, we explore the most essential accounting services for medical practices. We also provide a breakdown of specialized reports, financial metrics, and how a CPA firm can offer tailored support to help healthcare clients stay compliant, profitable, and efficient.
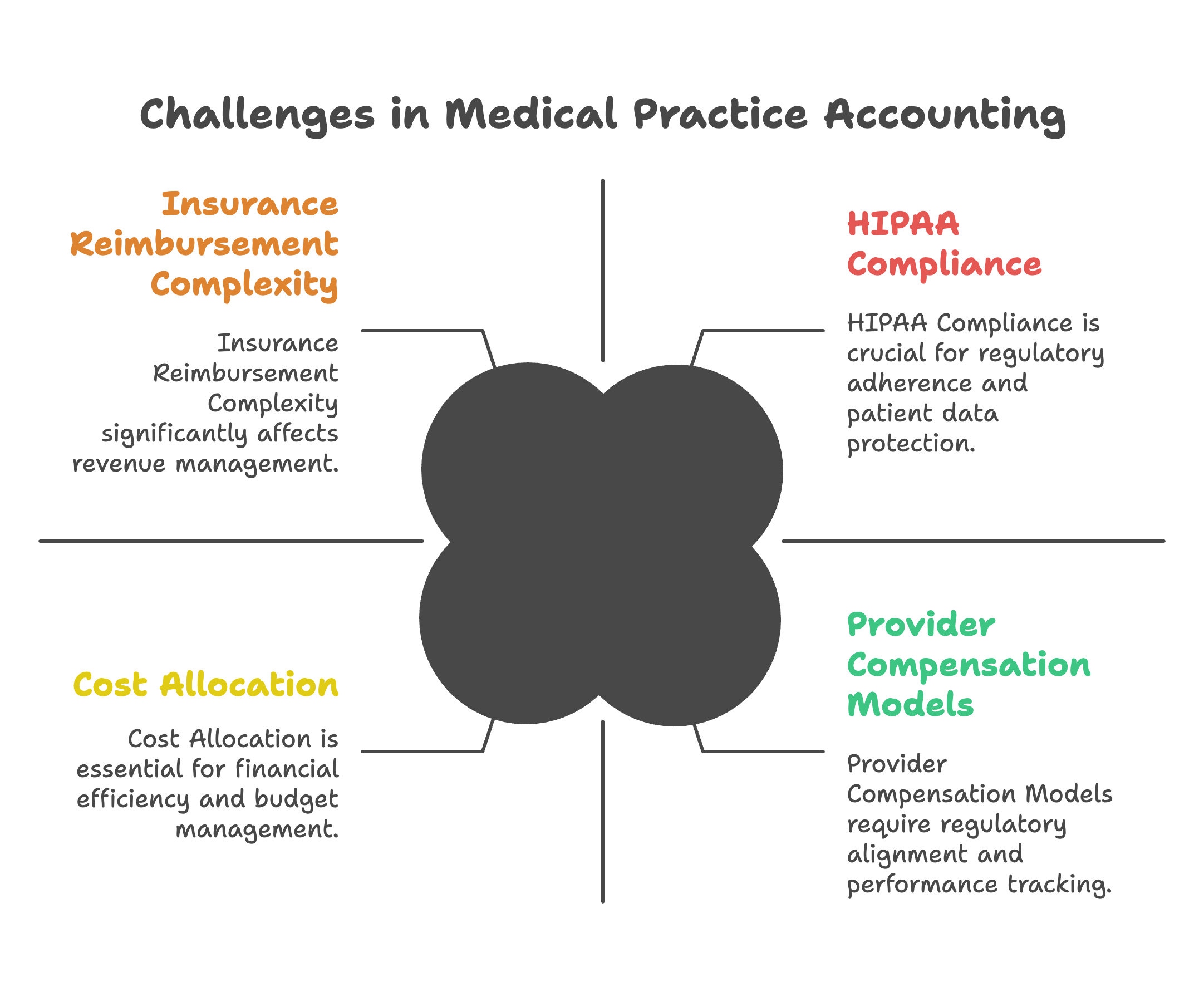
Medical practice accounting is not just about balancing revenue and expenses. It involves navigating HIPAA regulations, healthcare-specific tax issues, and variable billing cycles. Here are several reasons why general accounting services are insufficient for healthcare businesses:
Unlike retail businesses that get paid at the point of sale, medical practices deal with third-party reimbursements. Payments from Medicare, Medicaid, and private insurers arrive weeks after services are rendered and are often subject to adjustments, denials, or audits.
Medical practices generate income from various sources including insurance claims, copays, cash payments, lab services, referrals, and ancillary services. Tracking and reconciling these categories is critical for accurate reporting and requires specialized consultation to optimize revenue recognition.
Physician compensation may be based on salary, productivity, collections, profit-sharing, or a mix. Accounting systems must track performance metrics aligned with these contracts, often requiring ongoing consultation to ensure compliance and fairness.
HIPAA regulations impose strict requirements on handling financial records. Moreover, medical practices are subject to healthcare-specific tax codes and audits that require specialized knowledge from a qualified CPA.
Medical practices often share administrative costs, rent, and staff between departments or providers. Allocating these expenses fairly requires careful tracking and specialized reporting that can streamline operational decision-making.
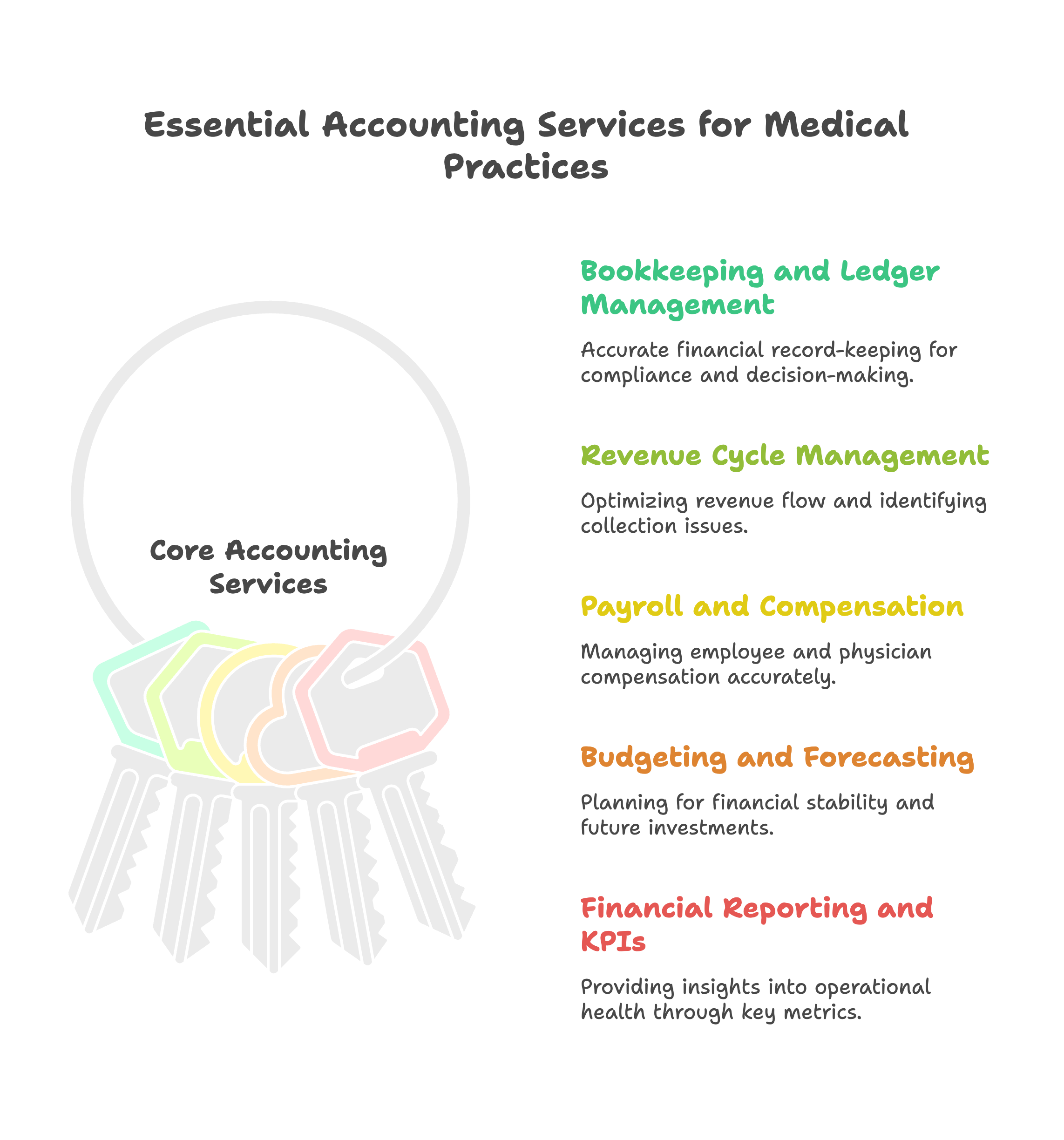
Accurate bookkeeping is the foundation of any medical practice accounting system. For medical practices, this involves:
Professional bookkeeping services ensure that healthcare professionals have accurate financial data for decision-making while maintaining compliance with industry standards.
Although medical practices usually rely on billing staff or third-party billers, a CPA can assist with revenue cycle oversight. This includes:
This consultation helps practices optimize their revenue cycle and improve cash flow timing.
Medical payroll goes beyond salary payments. Specialized accounting services for healthcare include:
For physicians, accounting services should track:
Budgeting is critical for medical practices, where reimbursements are delayed, but payroll and vendor payments are due regularly. Professional consultation in this area helps:
Medical practices need customized reports that help them understand operational health. Key reports include:
To assess financial and operational performance, medical practices should regularly monitor the following metrics:
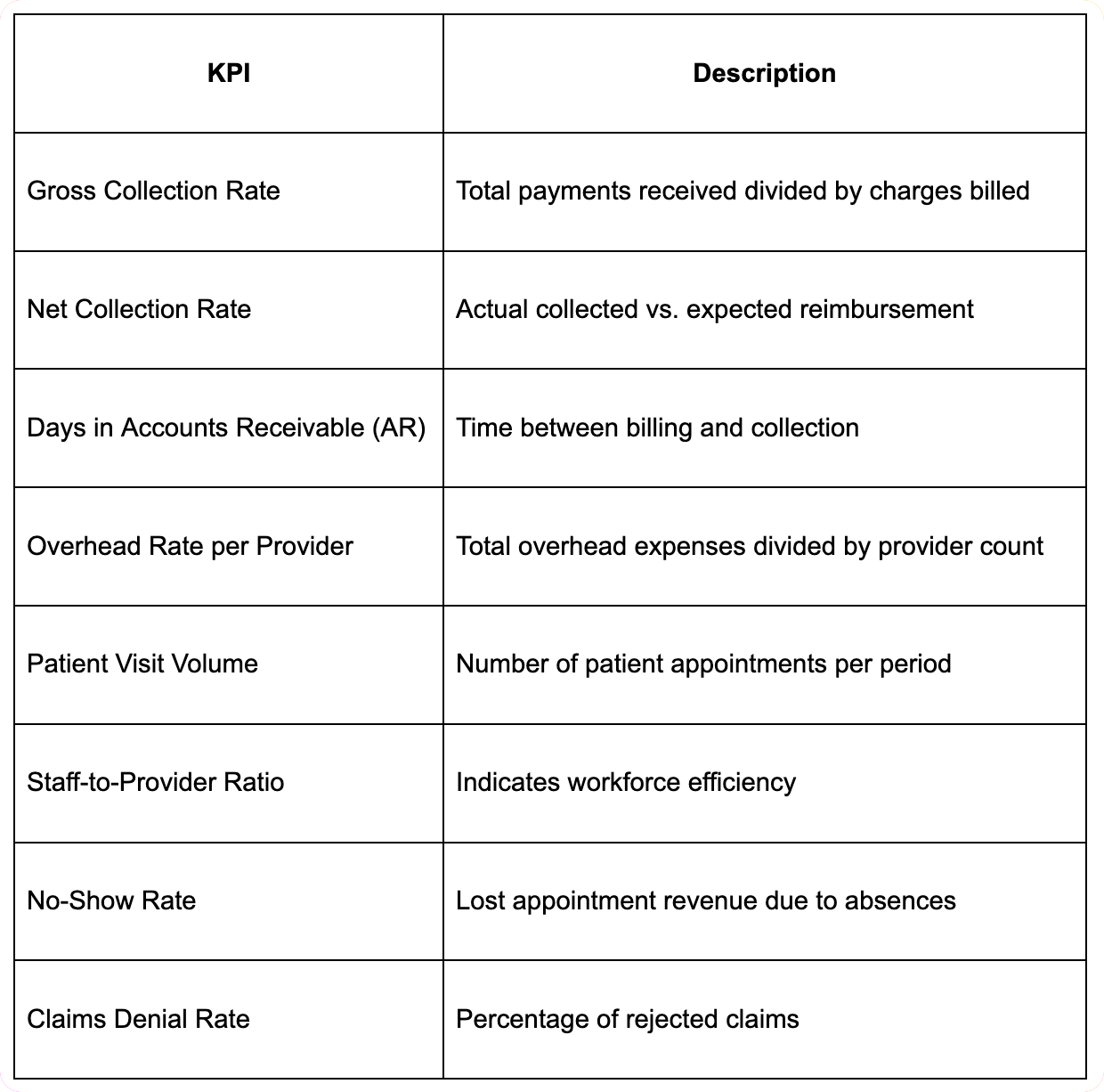
Tracking these metrics through specialized medical practice accounting helps identify trends, spot operational inefficiencies, and create accountability for healthcare professionals.
The choice between forming as a sole proprietorship, S corporation, partnership, or professional corporation can have significant tax implications for medical practices. Each structure affects:
A qualified CPA must evaluate the practice's size, income, and growth plans to recommend the right setup through comprehensive tax planning consultation.
High-value assets like X-ray machines, ultrasound devices, and EHR systems qualify for depreciation. Medical practices should use Section 179 or bonus depreciation strategies to reduce taxable income through strategic tax planning.
Some providers may qualify for the 20 percent QBI deduction under Section 199A. However, this benefit is subject to income limits and exclusions that affect service-based businesses like medicine. Accurate income tracking and specialized tax planning are essential.
Medical practices may qualify for tax credits such as the Employee Retention Credit (ERC) or paid leave credits. Navigating these opportunities requires CPA oversight and documentation support.
Choosing the right accounting software is essential for efficient operations. The best tools integrate with practice management software and EHR systems to streamline operations. Top options include:
An experienced accountant can add value beyond bookkeeping by offering specialized advisory services such as:
This consultation is important for buy-ins, retirements, or selling the business. A valuation considers:
Compare the practice's performance against similar organizations using industry standards for productivity, revenue, and efficiency through detailed consultation services.
Internal controls such as segregated duties, reconciliations, and audit trails protect medical practices from embezzlement or data manipulation.
Help practices prepare for the departure of a key provider through structured buyout models, tax-efficient sale structures, and operational handovers.
Many medical practices face the decision of whether to outsource their accounting functions or maintain in-house staff:
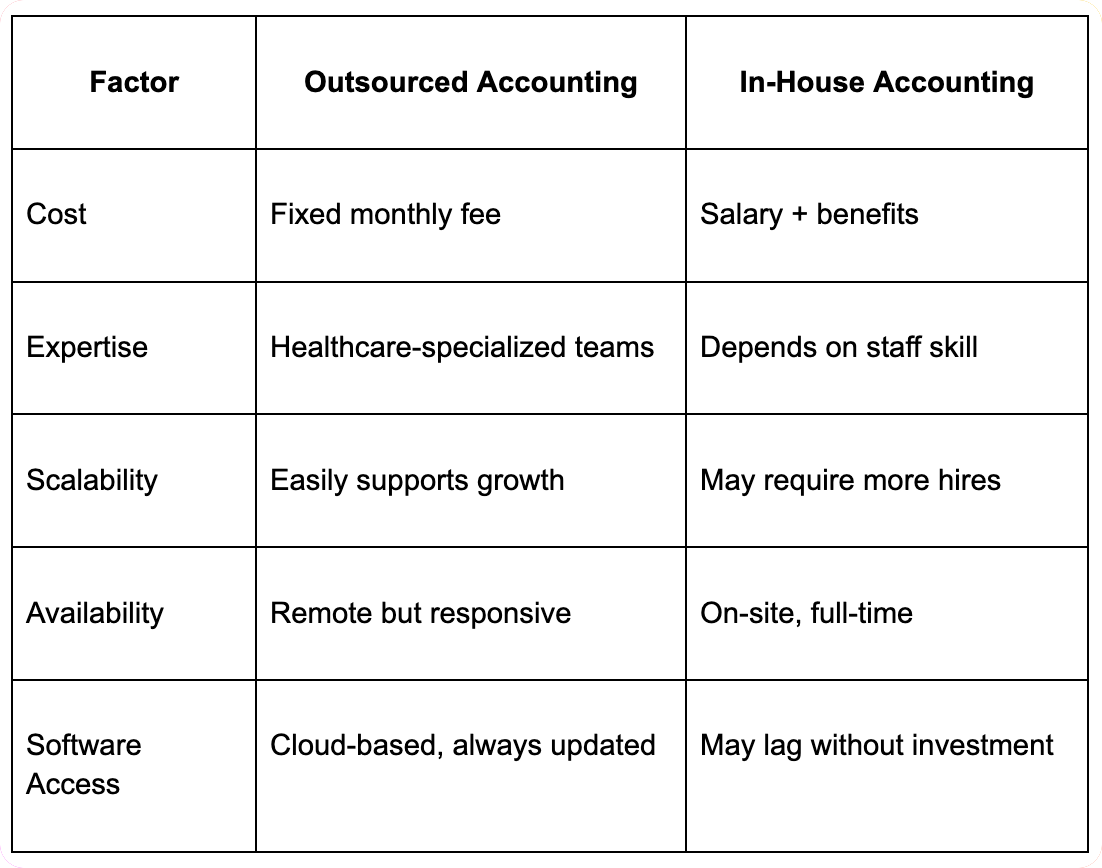
The decision to outsource often depends on practice size, complexity, and budget considerations. Many medical practices find that outsourced accounting services provide better expertise and cost efficiency.
When healthcare professionals can rely on expert accounting services, they can dedicate more time and attention to patient care rather than administrative burdens. Proper financial management supports the primary mission of medical practices.
Specialized medical practice accounting helps identify revenue opportunities, control costs, and optimize operational efficiency. This leads to better financial outcomes and practice sustainability.
Working with a CPA firm that understands healthcare regulations ensures compliance with complex requirements, reducing risk and protecting the practice's reputation.
Professional consultation services help medical practices plan for expansion, equipment purchases, and staffing changes based on solid financial analysis and forecasting.
Modern accounting services for medical practices should integrate seamlessly with EHR systems to:
Integration between accounting and practice management systems helps healthcare professionals:
Without expert accounting support, medical practices face several risks:
Preventing these issues requires monthly reconciliation, active CPA oversight, and use of medical-specific software that can streamline financial operations.
A CPA firm specializing in healthcare can provide consultation on:
Healthcare professionals benefit from consultation on:
Ongoing consultation helps medical practices stay current with:
The healthcare industry continues to embrace new technologies that can help medical practices:
As healthcare shifts toward value-based payment models, medical practices need accounting services that can:
Regular consultation with a qualified CPA helps medical practices:
Ongoing accounting services provide healthcare professionals with:
Accounting for medical practices requires specialized knowledge, dedicated systems, and ongoing support that goes far beyond traditional bookkeeping. The complexity of insurance reimbursements, regulatory compliance, and physician compensation models demands expertise that only a qualified CPA with healthcare experience can provide.
Medical practices that invest in professional accounting services and regular consultation can focus their energy on patient care while maintaining strong financial health. Whether through outsourced services or enhanced in-house capabilities, the right medical practice accounting approach helps healthcare professionals navigate the complex financial landscape of modern medicine.
A CPA firm specializing in healthcare can provide the tax planning, financial analysis, and strategic consultation needed to ensure long-term success. By partnering with accounting professionals who understand the unique challenges of the healthcare industry, medical practices can streamline their operations, optimize their financial performance, and concentrate on what matters most – providing excellent patient care.
Question: What specialized accounting services do medical practices need beyond general business accounting?
Answer: Medical practices require specialized accounting services including medical billing and coding support, insurance claim processing, accounts receivable management for patient and insurance payments, and compliance with healthcare regulations like HIPAA. Services include credentialing and payer enrollment assistance, prior authorization tracking, denial management, and patient payment processing. Additional needs cover medical equipment depreciation, malpractice insurance accounting, employee benefit plan management, and preparation for healthcare audits. Specialized software integration and reporting for medical practice management systems distinguish healthcare accounting from general business accounting services.
Question: How do medical practice revenue cycles differ from other businesses and what accounting considerations apply?
Answer: Medical practice revenue cycles involve complex processes with patient services, insurance claim submission, payment processing from multiple payers, and patient responsibility collection. Unlike traditional businesses with direct customer payments, medical practices deal with insurance companies, government programs, and patient co-pays creating extended collection periods and payment uncertainty. Accounting considerations include revenue recognition timing, allowance for doubtful accounts estimation, insurance contract analysis, and management of claims in various payment stages. Practices must track aging receivables by payer type, monitor denial rates, and manage cash flow despite extended payment cycles.
Question: What compliance and regulatory requirements affect medical practice accounting?
Answer: Medical practices face extensive compliance requirements including HIPAA privacy regulations affecting financial record handling, Medicare and Medicaid billing compliance, state insurance regulations, and fraud prevention measures. Anti-kickback statutes, Stark Law compliance, and corporate practice of medicine restrictions affect financial arrangements and reporting. Quality payment programs like MIPS require financial tracking and reporting for performance incentives. Practice accounting must support compliance monitoring, audit preparations, and documentation requirements for regulatory investigations. Professional liability insurance, credentialing requirements, and license maintenance also create accounting and reporting obligations.
Question: How should medical practices handle accounts receivable management and collection procedures?
Answer: Medical practices should implement systematic accounts receivable management including electronic claim submission, real-time eligibility verification, denial management procedures, and patient payment processing systems. Establish aging analysis by payer type, implement collection procedures for different account categories, and maintain compliance with fair debt collection practices. Use practice management software for automated follow-up, track key metrics like days in accounts receivable and collection rates by payer. Develop patient payment plans, implement point-of-service collection procedures, and consider professional collection services for aged accounts while maintaining HIPAA compliance.
Question: What financial reporting and analysis tools are most valuable for medical practices?
Answer: Valuable financial reporting for medical practices includes provider productivity analysis, payer mix reporting, procedure profitability analysis, and collection rate monitoring by payer and procedure type. Key reports cover accounts receivable aging, denial analysis, patient satisfaction correlation with financial metrics, and overhead cost analysis by department or provider. Dashboard reporting should include daily collections, outstanding claims status, appointment scheduling efficiency, and revenue per visit metrics. Comparative analysis against industry benchmarks and historical performance helps identify improvement opportunities and financial trends requiring management attention.
Question: How do medical practices optimize their billing processes and increase collections?
Answer: Optimize medical practice billing by implementing electronic health records with integrated billing, training staff on proper coding and documentation, establishing front-end eligibility verification, and using automated claim submission systems. Improve collections through point-of-service payment collection, patient payment plans, online payment portals, and prompt follow-up on denied claims. Monitor and improve clean claim rates, reduce days in accounts receivable, and implement systematic denial management procedures. Regular training on coding updates, payer policy changes, and compliance requirements helps maintain optimal billing performance and minimize revenue leakage.
Question: What technology solutions should medical practices consider for financial management?
Answer: Medical practices should consider integrated practice management systems combining scheduling, billing, and financial reporting, electronic health records with billing modules, and automated payment processing systems. Technology solutions include claims clearinghouses for electronic submission, patient portal systems for online payments, and business intelligence tools for financial analytics. Consider automated appointment reminders with payment collection, denial management software, and integration between clinical and financial systems. Cloud-based solutions offer scalability and security, while mobile applications enable remote access to financial information and patient account management.
Question: How can medical practices work effectively with specialized healthcare accounting firms?
Answer: Work effectively with healthcare accounting firms by providing access to practice management systems, maintaining organized financial records, and establishing regular communication schedules for financial reviews. Choose firms with medical practice expertise, knowledge of healthcare regulations, and experience with practice management software. Establish clear service expectations, reporting requirements, and communication protocols. Provide training on practice operations, payer requirements, and clinical workflow impacts on financial processes. Regular meetings should cover financial performance, compliance issues, and strategic planning for practice growth and optimization. Ensure accountants understand medical practice challenges and revenue cycle complexities.

A practical comparison of hiring a freelancer vs using a dedicated offshore accounting team, focusing on continuity, quality control, security, and scaling.
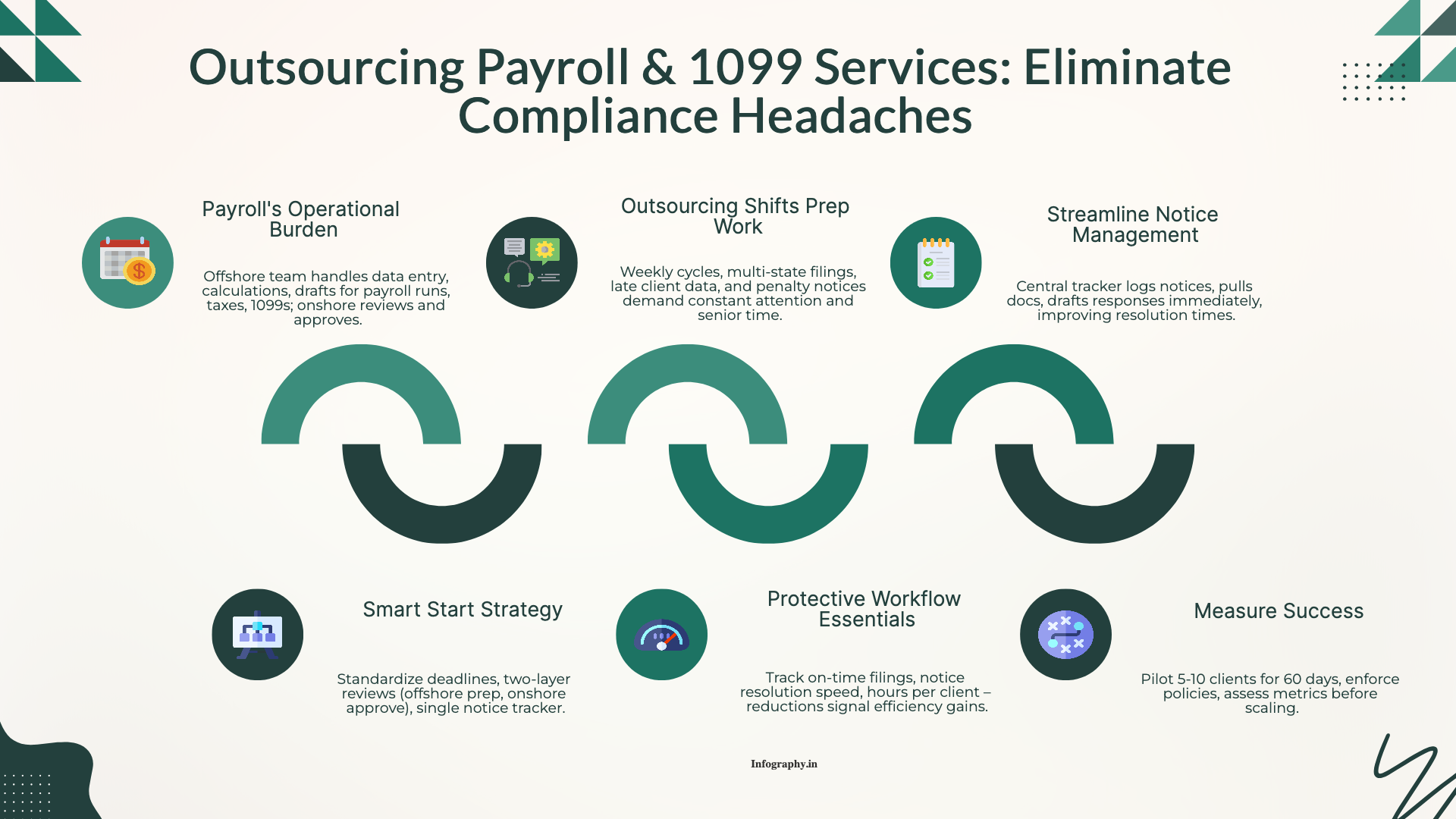
How CPA firms outsource payroll and 1099 work to reduce penalties and admin load, with a clean workflow for approvals, filings, and year-end reporting.
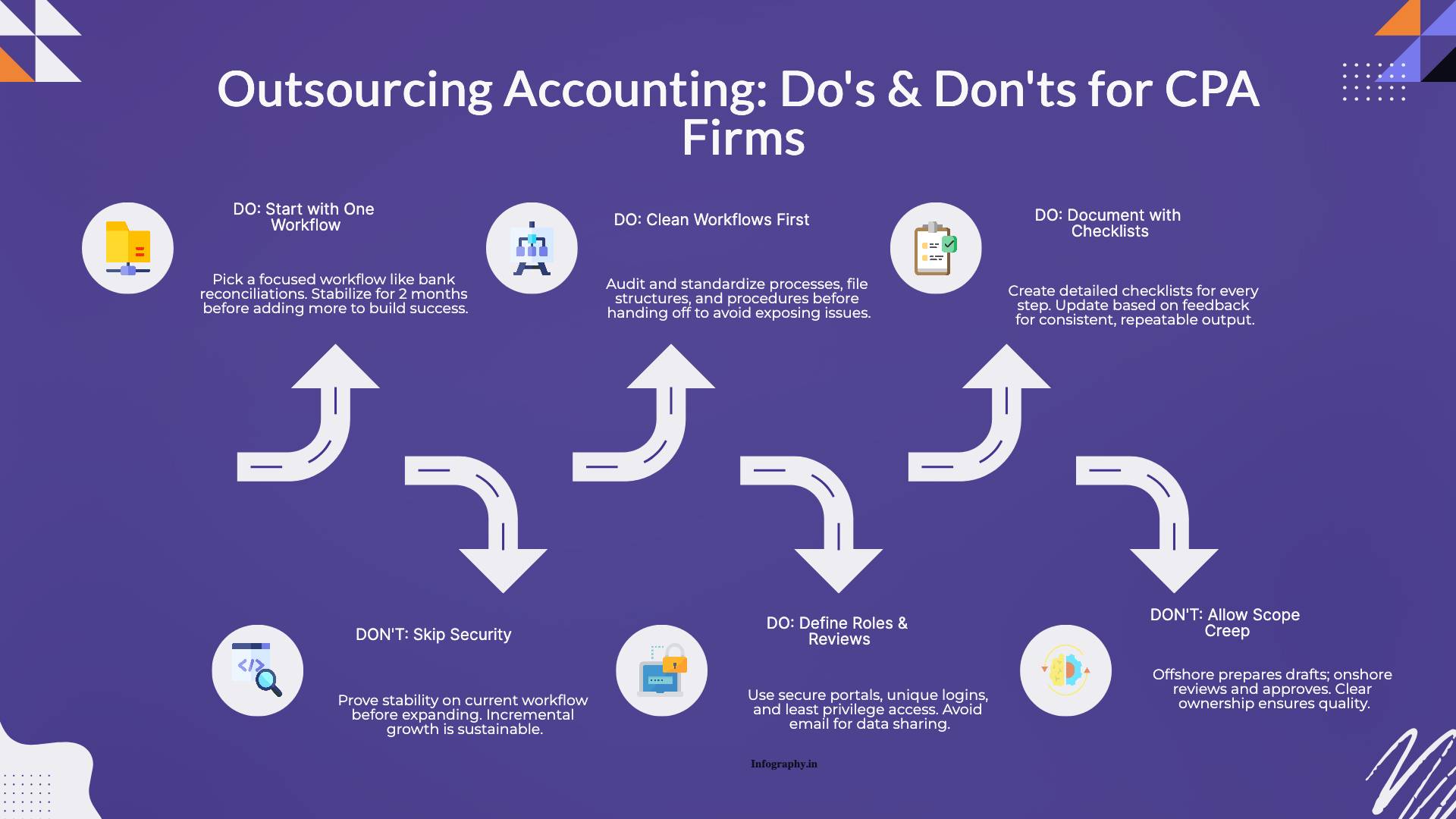
Practical do's and don'ts for CPA firms outsourcing accounting work, based on common failure points and what successful rollouts do differently.